For Vancouver resident Farrell Eckman, having a long conversation or attending a workout class without breaking into coughs is a major accomplishment.
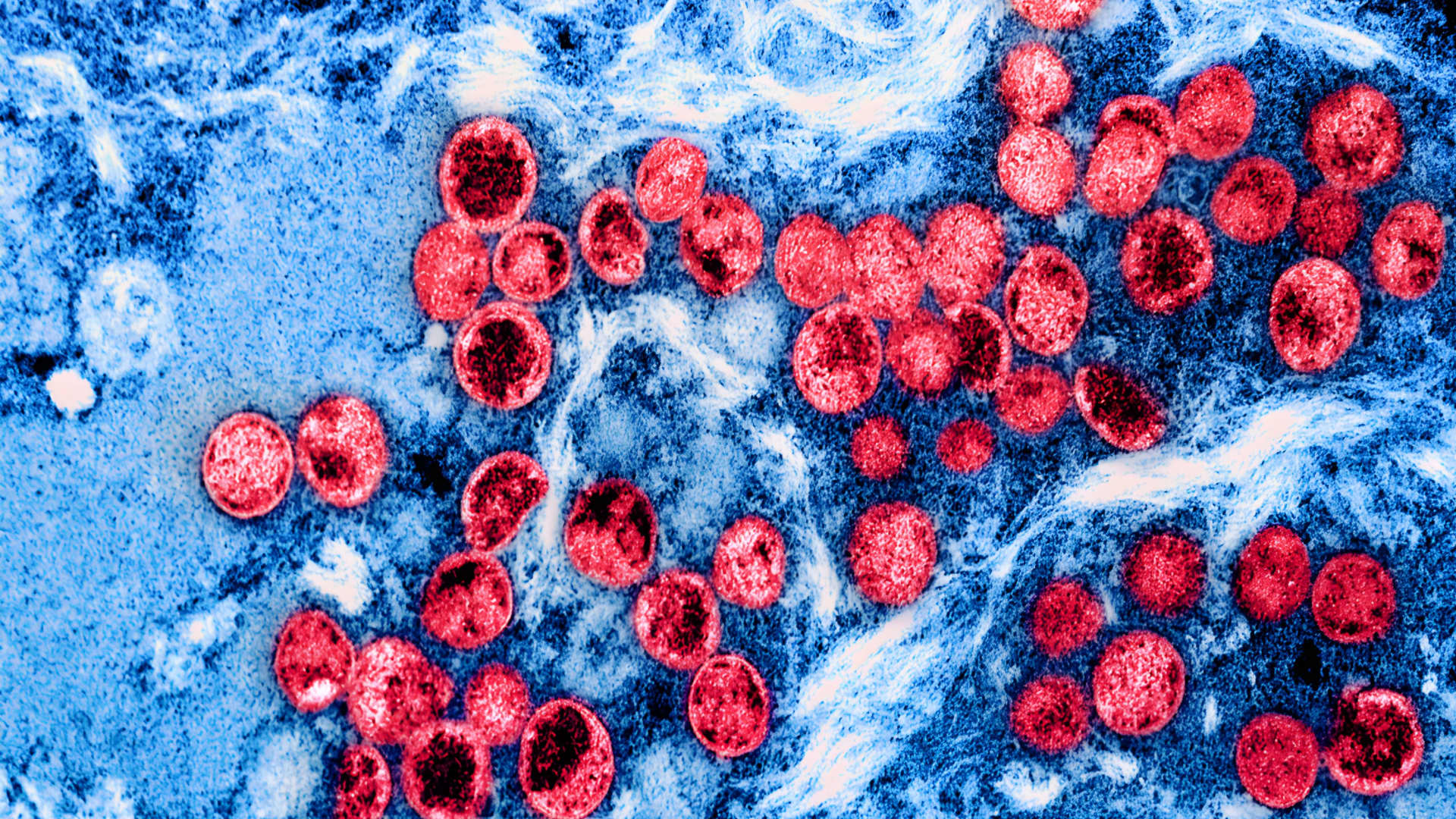
The 50-year-old is one of many people who researchers say developed pulmonary fibrosis — a condition that thickens the tissue in lungs and can affect breathing — after experiencing a severe case of COVID-19.
In January 2022, Eckman was admitted to Vancouver General Hospital because she was having trouble breathing along with flu-like symptoms.
“I spent over a month in ICU. I was on a ventilator. Not once, but twice. [My family] thought they were gonna lose me,” she recalled. “It was the scariest time we’ve ever been through.”

Eckman’s time in hospital was caused by her second bout of COVID. She had received three vaccines for the coronavirus that causes the disease.
While she eventually recovered and was released to go home along with six litres of oxygen, which is the maximum amount a patient can be discharged with. Eckman was later diagnosed with pulmonary fibrosis, caused by the toll that COVID took on her lungs.
“The damage that was sustained to my lungs from COVID pneumonia was severe. They’ve looked at my lungs numerous times. I don’t know if I’ll ever fully recover. I’m functioning, which is tremendous. But I could possibly be dealing with this for the rest of my life.”
A meta-analysis published in the Annals of Medicine & Surgery in April 2022 found almost 45 per cent of recovered COVID-19 patients developed pulmonary fibrosis, and those patients often suffered persistent symptoms such as coughing, chest pain and fatigue.
The research also drew a link between severity of COVID-19 symptoms and severity of consequent pulmonary fibrosis.
It’s something Daniel Marinescu, a respirologist at Vancouver General Hospital, says he is seeing more often, adding that patients are more prone to developing pulmonary fibrosis depending on how severe scarring of their lung tissue is.

Marinescu says he’s seen “several dozen” of these cases.
“Most of the time it is a fairly mild disease and most of the time people slowly get better over months and years,” he said. “But sometimes people take a big hit if they’re in the ICU for a long time or on the ventilator for a long time.”
Janet Pope, a rheumatologist and professor of medicine at Western University in London, Ont., says while research is limited, factors like age and smoking could affect the likelihood of patients developing the condition.
“We know that COVID pneumonia can cause pulmonary fibrosis. Not in most people who get COVID pneumonia, but if it’s more severe, older age groups, more severe inflammation of the lungs from COVID,” she said.
Pope adds patients may feel frustrated with their symptoms, but recommends sharing concerns with health-care professionals.
“They would take a stethoscope and listen to the bottom of the lungs. It takes four seconds to do. If they hear what we call ‘crackles’ then they can do a chest X-ray,” she said.
“Have a listen to people if they say they’re short of breath, if they’re coughing, if they have a cold that’s not improving,” she advises.
For Eckman, recovery remains a constant in her life. She says she works daily on improving her breathing, and does pilates regularly. However, she still occasionally has to use oxygen at night to help with her breathing.
“I just passed my two-year anniversary. I’m still dealing with it. It’s an ongoing process,” she said.