Dr. Sarah Giles got hooked on rural medicine by spending a summer volunteering in the Northwest Territories.
Giles, who was still a student at the time, flew in and out of seven different communities, providing care “with the most amazing doctor ever.”
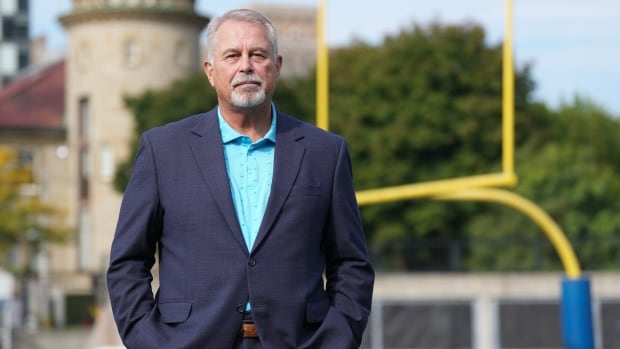
“I thought to myself, ‘This is real medicine. This is what I want to do,'” said the doctor, a former board member of the Society of Rural Physicians of Canada who now lives and works in Kenora, Ont.
As rural health-care facilities in Manitoba, Canada and across the country struggle to find staff to keep their services running, Giles and Dr. Sarah Newbery offered their insights on how they might overcome those problems.

Some small southwestern Manitoba communities, including Killarney, Hamiota and Glenboro, have resorted to paying tens of thousands of dollars to a recruiting firm for successfully finding doctors who will work in their communities for at least four years.
Giles said recruiting firms can help with the precarious situation in some areas, but “robbing Peter to pay Paul” isn’t a long-term solution.
“I think everyone needs to understand that there’s a very, very small pool of recruitable rural doctors,” she said.
“It’s horrendous, but I firmly believe that our health-care systems in rural communities are going to see much darker days before things improve.”
Attract students as future doctors
The best way to find rural doctors who will stay is to have rural medical students, she said, but there’s a lot working against that.
Medical schools are in cities, and the people most likely to attend them are affluent people from cities, she said.
Giles is originally from Toronto, but that experience in the Northwest Territories and years in rural areas doing locum work — filling in for other physicians — ended with her taking a permanent position in Kenora.
Helping less affluent people from rural areas attend university in return for rural service when they’re doctors could help provide a long-term solution.
“If your community needs doctors, look at your high school students. Who of them could potentially be that rural doctor?”
If that’s not an option, there are ways to make it easier for doctors to relocate, such as helping them find appropriate housing and child care, making sure demands aren’t unrealistic and offering flexibility in how their practice is managed.
It can also include minimizing paperwork and making sure there’s help from other health-care providers, such as physiotherapists and nurse practitioners.
“The stress and the weight that is put on physicians is just not sustainable,” Giles said.

Newbery, a general family physician in Marathon, Ont., on the north shore of Lake Superior, said Canada’s physician shortage is actually improving — but that doesn’t seem to be helping rural areas.
“We do have fewer physicians per capita than other countries do, but we have more now than we’ve had in a long time,” said Newbery, who’s also the associate dean of physician workforce strategy at the Northern Ontario School of Medicine in Thunder Bay, Ont.
“It’s actually a distribution problem.”
Changing nature of the job
Many doctors are no longer providing comprehensive family medicine, she said — they’re specializing. Even fewer are choosing rural generalist practice, which generally entails working part-time in a clinic and also taking shifts at the local hospital.
Part of the problem is that the job has become more complex, both in patient care and administration, she said.
For example, different health-care facilities might use different electronic record-keeping systems, so a doctor might simplify the paperwork by practising in just one place, instead of doing a couple of days a week at a medical clinic and other days at a hospital and a long-term care home.
Retention is also an important part of the puzzle, Newbery said, urging communities to think creatively when it comes to keeping their doctors.
“Maybe somebody’s going to bring them meals three nights a week,” she said.
“They want to feel like they’ve got some work-life balance. They want to feel supported and they want to feel connected to the community.”
Feeling appreciated
While traditionally, rural doctors were men with wives at home taking care of their family lives, now 70 per cent of graduates from family medicine programs are women, she said, so quality child care should also be considered.
Having a great health-care team, with support from people like nurses and technicians, also has an impact, she said.
“Thank-you letters to team members and local physicians matter. Those nods of appreciation are valuable things.”
Giles echoed that, saying she actually got more thank-you letters from patients before the COVID pandemic than she does now.
“When you’ve been working over and above what you should, it is nice to hear the thank yous and the stories,” she said.
“One of my patients recently knit me a pair of socks.… You know, that will keep me going for a good six months.”